Overview
Contents in this page
What is Antimicrobial Resistance?
Antimicrobial resistance (AMR) refers to the ability of microorganisms (such as bacteria, viruses, fungi, and parasites) to continue to live or grow in the presence of drugs that were originally meant to kill or inhibit them.
AMR is a natural process that happens over time through genetic changes in microorganisms. We cannot stop microorganisms from becoming resistant, but we can slow down the process.
The spread of AMR has been accelerated by human activity, mainly through the misuse of antimicrobials. Antimicrobials include antibiotics, antivirals, antifungals, and antiparasitics.
What happens if microorganisms develop resistance?
Microorganisms that develop resistance to drugs meant to kill or inhibit them are sometimes referred to as ‘superbugs’. They can be found in people, animals, food, and the environment (e.g. water and soil).
Diseases in people and animals, caused by AMR-resistant infections, become very difficult or impossible to treat and make other medical procedures and treatments riskier.
This increases the risk of disease spread, severe illness, disability, and death.
In addition, drug-resistant infections impact animal and plant health, reduce farm production and productivity, and threaten food security.
How do we stop the AMR microoganisms from spreading?
Food producers, consumers and government agencies must work collectively to stop or slow down the spread of AMR microorganisms to ensure food safety.
Farmers
How do our farmers help combat AMR?
The fight against antimicrobial resistance begins with you!
Antimicrobials, which come in the form of antibacterials, antivirals, antiparasitic agents, and antifungals, are used to kill and slow the spread of microorganisms in farm animals.
When antimicrobials are used irresponsibly in food animals, the disease-causing microorganisms in the animals develop resistance and turn into microorganisms that are highly resistant to drugs meant to kill or inhibit them.
This makes disease outbreaks in farms very hard and expensive to treat, and also increases the risk of the disease spreading to other animals and into the food chain.
Use the resources below to learn how you, as a farmer, can play your part in slowing the rise of antimicrobial resistance in food animals and ensure that the food you produce is safe for all Singaporeans.
Combatting Antimicrobial Resistance on a Coastal Fish Farm
Watch the video to learn how to properly use antibiotics, antivirals, antifungals, and antiparasitics safely on your farm.
Veterinary Drug Residues in Food
Find out how you can reduce our exposure to veterinary drugs in food.
Veterinary Drug Residues in Food
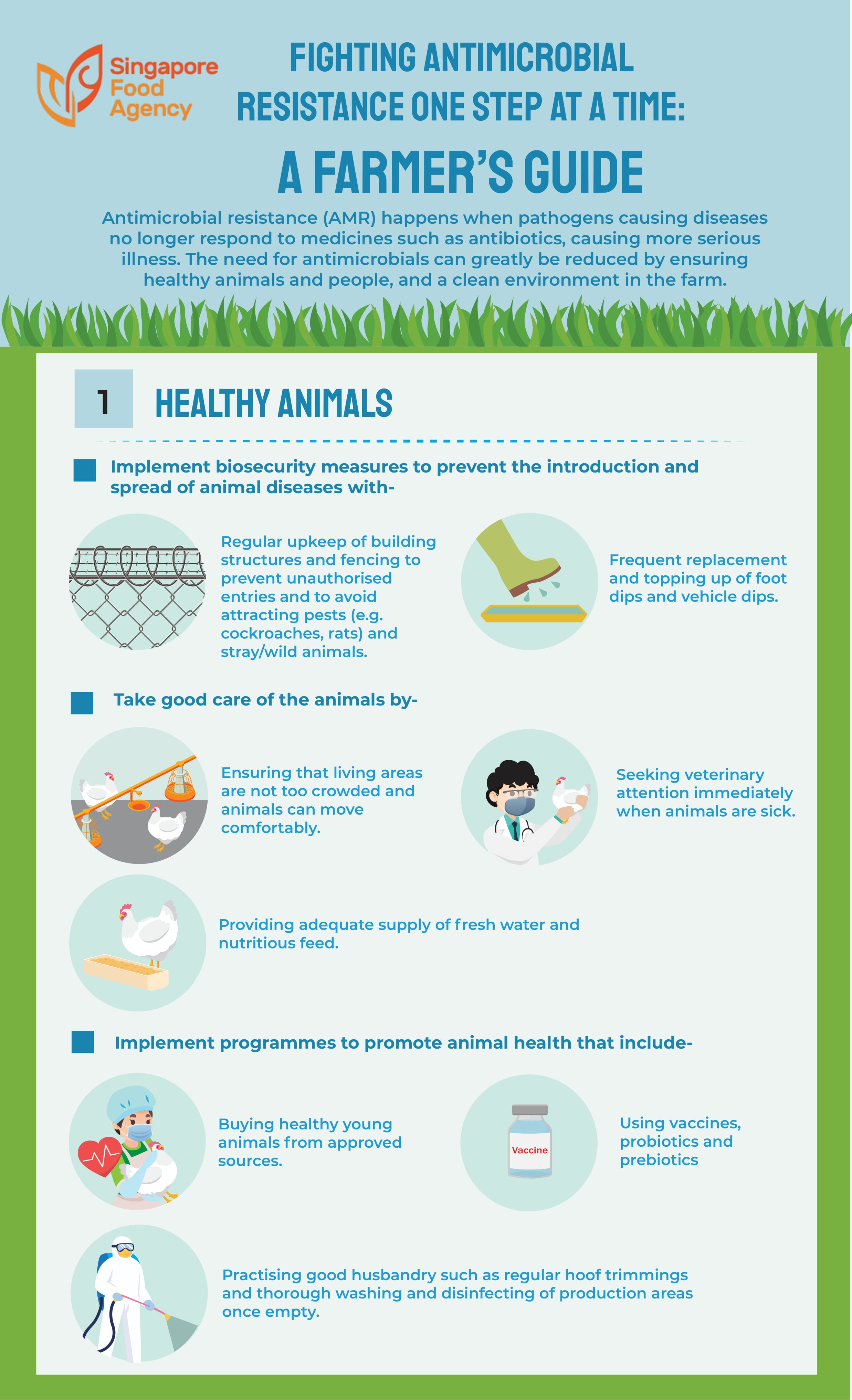
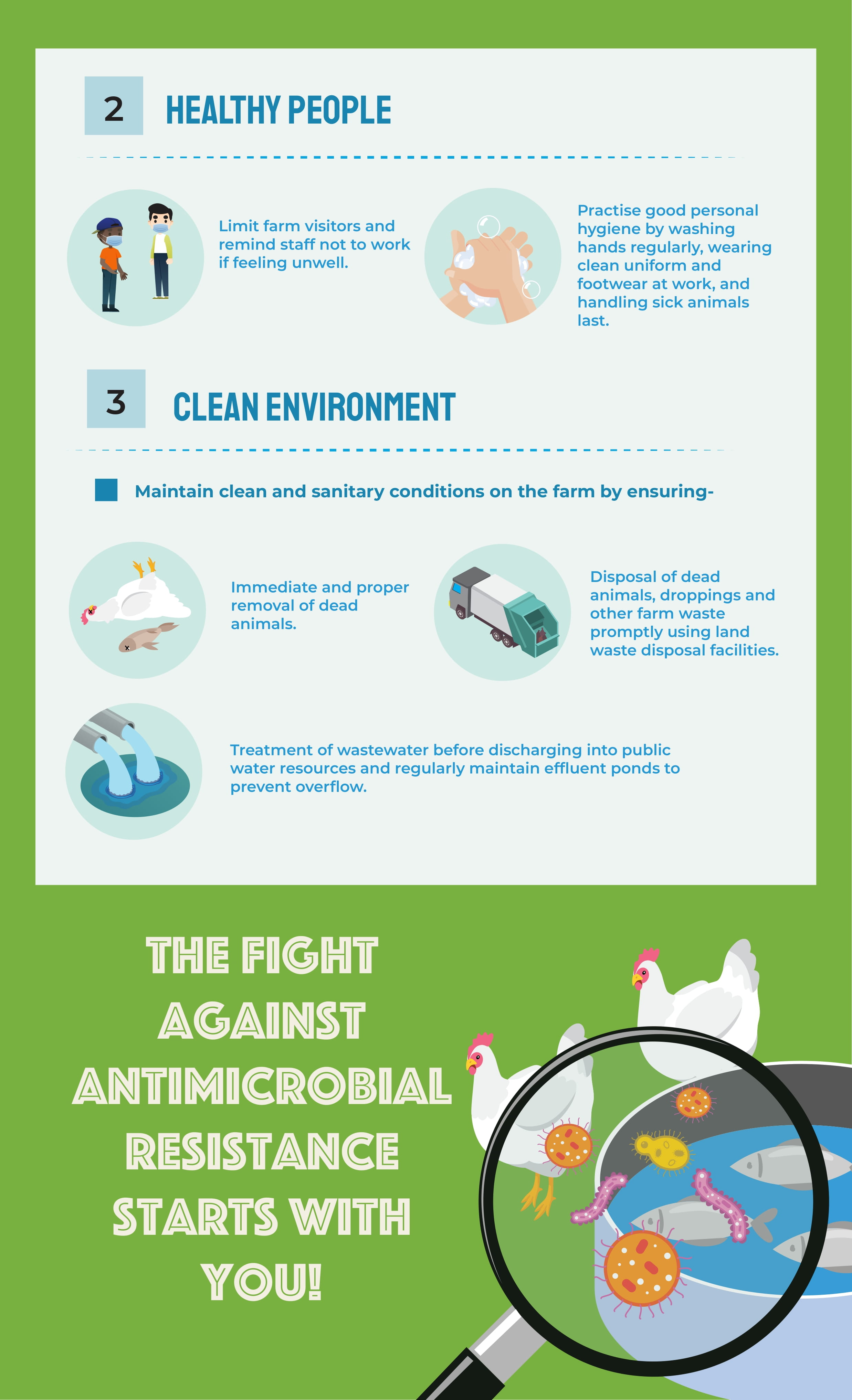
Fighting Antimicrobial Resistance One Step At A Time: A Farmer's Guide
Download the infographic below and follow the tips for healthy animals, healthy people, and a clean environment.
Fighting Antimicrobial Resistance One Step At A Time: A Farmer's Guide
 |  |
Consumers
How can consumers play their part?
Food can be contaminated at any point along the food chain. While SFA remains vigilant and works to ensure that regulatory measures are in place and properly enforced, the food industry and consumers can also play a part to ensure food safety.
Below are 5 ways you can help stop the spread of AMR.
1. Practise food safety
2. Cook food thoroughly
3. Prevent the spread
4. Buy from safe sources
5. Learn more about AMR
Government
Contents in this page
What is the Singapore government’s response to AMR?
AMR is a serious threat to global public health. It requires a multi-sectoral and multi-disciplinary approach to tackle the problem, as antimicrobial-resistant microorganisms can be transmitted through the food supply chain, the environment, and direct contact between animals and humans.
Whole-of-Government, One Health Approach
Recognising the serious threat AMR poses, Singapore has adopted a comprehensive One Health approach. It is a coordinated effort involving the animal, human, food, and environmental sectors.
This Whole-of-Government effort led to the development and launch of the One Health Master Plan in 2025 which serves as a national strategic plan to safeguard public health, and the National Strategic Action Plan on Antimicrobial Resistance Version 2.

The plan provides a framework to strengthen and enhance activities to combat AMR across the human, animal, food, and environmental sectors.
It is aligned with the World Health Organization's (WHO) Global Action Plan on AMR, as well as the standards and guidelines established by intergovernmental bodies such as the Food and Agriculture Organization of the United Nations (FAO) and the World Organisation for Animal Health (OIE).
Agencies involved in the National Strategic Action Plan on AMR
The National Strategic Action Plan on AMR (2017) was developed by:
- Ministry of Health (MOH)
- National Environment Agency (NEA)
- Former Agri-food & Veterinary Authority of Singapore (AVA)
(SFA was formed in April 2019 and consolidated food-related functions, including from the former AVA) - Public Utilities Board (PUB)
How does SFA combat AMR?
SFA has in place a food safety system based on science and risk analysis. All food products (both imported and locally produced) are required to comply with our food safety standards and requirements.
Working with local farms on antibiotic use
Regular inspections and sampling
Monitoring food-borne pathogens
Accreditation and certification schemes
Outreach and publicity
SFA’s regional role
FAQs
FAQs
Can humans become resistant to medicines?
Is eating meat from animals treated with antibiotics harmful?
Why do we not see ‘antibiotic-free’ food products in Singapore?
Will banning antibiotic use stop the increase in AMR?
For more information about AMR
You can access resources by local government agencies and global organisations by clicking on the links below:
Local government
Health Promotion Board (HPB): AMR
Health Promotion Board (HPB): Misuse of Antibiotics
National Parks Board (NParks): AMR
National Centre for Infectious Diseases (NCID): Antimicrobial Resistance Coordinating Office
Communicable Diseases Agency : One Health
Global organisations
Food and Agriculture Organization (FAO): AMR
World Health Organization: AMR
World Organization for Animal Health (OIE): AMR
World Organization for Animal Health (OIE): Farmers
You can also contact us through the SFA Online Feedback Form.